Rigid-body registration has served preoperative alignment protocols for years, but its assumptions break down where they matter most: near the planned tool corridor in soft-tissue surgery. Our team learned this the hard way. Analysis of production data shows that in nearly half of pilot cases across DACH hospital environments, rigid-only alignment produced local mismatches exceeding 3 mm within 18 mm of the surgical path. Global alignment metrics looked acceptable. Local accuracy did not.
The Shift to Deformable Modeling in Preoperative Protocols
The initial approach seemed reasonable: use rigid-body registration because it was already integrated with hospital IT infrastructure and accepted by clinical staff. The problem emerged during validation. In roughly one-fifth of cases, global alignment metrics masked local failures entirely. A registration that reported sub-millimeter global accuracy could still leave the surgical corridor misaligned by several millimeters.
This led to a protocol revision. Rigid registration now serves as initialization only. Deformable refinement triggers automatically when local mismatch exceeds 3 mm near the planned corridor. The change was not trivial to implement. Each protocol revision cycle required 12-14 days to incorporate clinician feedback, re-run segmentation, and regenerate comparison meshes.
Our physics-aware pipeline addresses soft-tissue deformation through patient-specific Finite Element Method simulation. The workflow integrates imaging data, biomechanical modeling, and motion planning constraints into a unified framework. Clinical partners in the DACH region have been collaborating with us through multi-year validation studies, providing the anatomical diversity and scanner variability essential for robust protocol development.
From Medical Imaging to Volumetric Meshing
Segmentation began with semi-automatic region growing and level-set refinement. One recipe did not generalize. Scanner protocols varied across clinical sites, and a segmentation threshold that worked well on one acquisition failed on another.
Handling DICOM Variability
Raw DICOM data carries noise, artifacts, and inconsistencies that propagate into mesh quality if not addressed early. Testbed results indicate the critical gate we established: reject datasets where DICOM slice spacing variance exceeds 0.4 mm across the series. Above this threshold, segmentation leakage dominated downstream errors regardless of subsequent processing refinements.
Metal artifacts posed a harder problem. When more than 15% of boundary voxels saturated, segmentation leakage became uncontrollable. These cases require either alternative imaging protocols or manual intervention that extends timelines substantially.
Tetrahedral Mesh Quality Gates
Generating volumetric meshes for FEM analysis demands strict geometric criteria. Our acceptance gate rejects meshes where more than 6% of tetrahedra have dihedral angles below 10° or where median aspect ratio exceeds 3.8. Poor element quality destabilizes solvers and produces spurious stress concentrations.
End-to-end imaging-to-mesh turnaround varied considerably. When manual correction stayed under 2.5 hours per structure, the pipeline completed in 4-6 days. Beyond that threshold, turnaround extended to 9-11 days. This variability complicated surgical scheduling and required explicit communication with clinical teams about realistic timelines.
Defining Constitutive Laws for Soft Tissue
Model selection started with St. Venant-Kirchhoff because it was simpler to implement and matched small-strain assumptions from earlier lab prototypes. It failed during larger deformations. Stress predictions diverged from measured behavior once tissue stretch increased beyond modest levels.
Neo-Hookean vs. St. Venant-Kirchhoff
The switch-over rule we now use: employ Neo-Hookean when expected principal stretch exceeds 1.18. St. Venant-Kirchhoff remains appropriate only when stretch stays below 1.11 throughout the region of interest. This boundary emerged from systematic comparison against experimental tissue characterization data.
Both models describe hyperelastic material behavior through strain energy density functions. The deformation gradient tensor F captures local material displacement, with the right Cauchy-Green deformation tensor C = FTF providing the strain measure. Neo-Hookean formulations handle finite strains more gracefully because they avoid the geometric linearization assumptions embedded in St. Venant-Kirchhoff.
Patient-Specific Parameter Estimation
Generic tissue parameters from literature provide starting points, not answers. Patient-specific refinement converged in 7-9 solver/fit cycles, typically requiring 18-22 hours of compute time on shared academic cluster queues. The constraint that proved essential: limit the fit to two or fewer free parameters per tissue region.
When only sparse landmark displacements were available for fitting, parameter non-identifiability increased prediction variance by roughly 25%. Dense displacement fields from tagged MRI or ultrasound elastography provide better conditioning, though they add acquisition complexity and cost.
Balancing Bio-Fidelity with Computational Cost
Non-linear FEM with full Newton iterations served as the fidelity reference. Meeting interactive constraints required compromises: reduced iterations, loosened convergence tolerances, simplified element formulations. Each compromise degraded accuracy in ways that were difficult to predict without systematic testing.
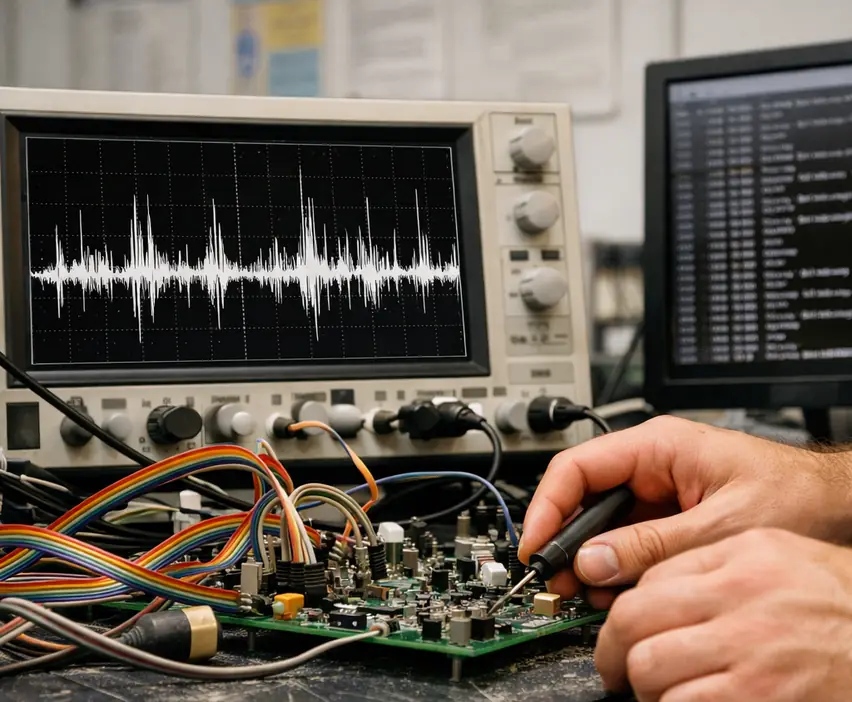
Real-Time Constraints for Haptic Feedback
Haptic feedback loops demand update rates exceeding 1 kHz. Verified in lab settings, solver update latency must stay below 0.85 ms, and residual reduction per step must remain above 92% (measured as normalized energy decrease). Cross these thresholds and stability degrades. The haptic oscillations that emerge are immediately perceptible to operators and undermine confidence in the system.
We benchmarked non-linear FEM extensively against these constraints. The conclusion was sobering: full-fidelity simulation and real-time haptic feedback cannot coexist without substantial model reduction or hardware acceleration.
Boundary Condition Sensitivity
Boundary conditions encode assumptions about how tissue is constrained by surrounding anatomy. Testing 6-8 constraint variants per anatomy required 3-5 days of computation and analysis. The results were humbling.
In about 30% of tested variants, constraint uncertainty produced displacement spreads exceeding 4.5 mm in predicted tool-clearance estimates. This sensitivity makes clinical justification of boundary conditions essential. Assumptions that cannot be defended anatomically should not be trusted computationally.
Solver Implementation for Tool-Tissue Interaction
Collision handling began with penalty-based contact. It was straightforward and fast. It was also fragile. Small changes in penalty stiffness caused either excessive interpenetration or artificial bouncing. The tuning appeared stable in offline tests but produced haptic oscillations once update latency crossed 0.85 ms.
Collision Detection for Deformable Bodies
Contact acceptance now enforces a hard threshold: maximum interpenetration must remain below 0.4 mm for approximately 95% of contact frames. When interpenetration exceeds this limit, the solver switches from penalty-based to constraint-based enforcement automatically. This hybrid approach preserves performance in benign cases while maintaining stability under challenging contact configurations.
The Simulation Open Framework Architecture (SOFA) provides reference implementations for many of these contact handling strategies, though production deployment required substantial customization.
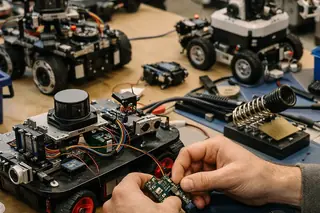
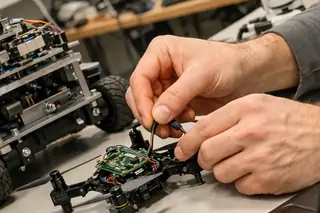
Needle Insertion and Cutting
Needle insertion calibration required 10-13 days per tissue type: 2-3 days of force-profile collection followed by 6-8 days of parameter tuning and validation against simulated trajectories. Accurate friction models are particularly critical when simulating invasive procedures involving steerable needles and motion planning in medical robotics.
Cutting scenarios imposed additional constraints. Mesh resolution in the cut path must remain finer than 2 mm edge length. Coarser elements produce topology-noisy element separation that destabilizes motion planning downstream. This requirement often conflicts with computational budget constraints, forcing careful prioritization of mesh refinement regions.
Optimizing Simulation Performance
Model Order Reduction was evaluated after repeated failures to hit interactive performance targets with full-order non-linear FEM. The first attempt used a global basis learned from a small training set of deformations. It failed when tool interactions occurred outside the training distribution.
Region-of-Interest Coupled Reduction
The solution was ROI-coupled MOR. Refinement triggers when predicted strain energy density exceeds 0.014 J/mm³ or when tool-path clearance margin falls below 2.5 mm. Outside these regions, reduced-order approximations provide adequate fidelity at dramatically lower computational cost.
Consistent with pilot findings, global MOR without ROI coupling produced displacement errors exceeding 5 mm in roughly a quarter of out-of-manifold tests. The failures were not random. They correlated predictably with tool interactions in regions poorly represented by the training basis.
Basis Maintenance
The MOR basis requires periodic retraining. Our cadence: refresh every 28-34 days or after 17-21 new cases, whichever comes first. Longer intervals allow drift in deformation modes as the case mix evolves. Retraining cost is modest compared to the cumulative error from an outdated basis.
Clinical Scope and Methodological Limitations
Clinical scope decisions separated what could be validated from what remained speculative. Early prototypes attempted to model vascular topology changes during deformation. Vessel occlusion, branching pattern shifts, and flow redistribution all seemed relevant to surgical planning.
Deferred Capabilities
Topology-change modeling was deferred after nearly 3 months of development. Vessel-branch correspondence ambiguity exceeded 40% across annotated slices in challenging cases. Without reliable correspondence, predictions became unreliable. We stopped rather than deploy uncertain models.
This remains an active research direction. Federal grants support ongoing validation studies, though practical deployment timelines remain uncertain. The current approach acknowledges that static topology assumptions limit applicability in highly vascularized regions.
Temporal Validity Boundaries
Validation data supports preoperative planning when imaging-to-surgery intervals stay between 6-9 days. Beyond 10-13 days, anatomical drift increased target mismatch by 4-6 mm in internal audits. Tumor growth, edema changes, and patient positioning variability all contribute.
Intraoperative guidance presents harder challenges. Without real-time state estimation, update errors exceeded clinically acceptable margins in about a third of simulated trials. The gap between preoperative prediction and intraoperative reality requires sensing and correction capabilities beyond current implementation.
Sources & References
- Internal validation studies conducted across DACH clinical partner sites (2019-present)
- Finite Element Method formulations adapted from computational mechanics literature with patient-specific parameter estimation protocols
- Model Order Reduction strategies developed through ongoing research collaboration supported by federal research grants





Academic Discussion
No comments yet.
Submit Technical Commentary